As students return to campus for Fall classes, UF is approaching a seven-day case average peak comparable to January, which was one of the largest since the start of the COVID-19 pandemic.
The wave in cases is expected to keep growing — UF researchers project the Delta outbreak to peak in late August or September. UF Health Shands Hospital has more COVID-19 patients now than ever, pushing the hospital to postpone certain elective procedures for the second time. The number of patients 19 years old and younger in the intensive care unit for the virus is higher than ever before.
“I don’t see an end in sight,” Shands CEO Ed Jimenez said. “If it’s true that we’re not peaking yet, then there’s more to come — that’s nerve-racking.”
The report from UF biostatisticians predicted the peak would take place over the first three weeks of Fall classes at UF — projecting to reach 33,000 reported cases per day and 220,000 per week in Florida.
As of Aug. 17, Florida’s highest number of weekly cases during the pandemic was over summer, with over 151,000 cases reported for Aug. 6 to 12.
From Aug. 8 to 13, UF reported 141 positive tests and a record-breaking 1,512 people in quarantine or isolation as of Tuesday. UF no longer provides on-campus quarantine or isolation spaces for students.
Burdened with coronavirus patients, Shands announced in an email Aug. 9 that elective procedures requiring an overnight stay must be postponed. This is the second order to limit elective procedures after Shands announced the week prior that all elective surgeries requiring an ICU stay would be postponed.
Canceling these procedures gives the hospital flexibility to adapt to increasing COVID-19 patients, Jimenez said.
Shands COVID-19 hospitalizations broke records again Aug. 9 with 216 patient beds occupied and 41 patients in the ICU. Of the total patients hospitalized, 94% were unvaccinated, Jimenez said.
As of Aug. 12, Shands had 215 patients, which he said looks like stability, but patients are getting sicker faster as the number of ICU patients climbed by 13 adults.
Because of higher viral loads, Jimenez said the Delta variant is more infectious than other strains.
In addition to the adult ICU patients, six children were staying in Shand’s ICU due to COVID-19 infection Aug. 12 — the hospital’s highest number of minors in the ICU for the virus since the start of the pandemic, Jimenez said.
“We’ve had at least one kid in the ICU every single day in the last month,” he said. “Back in our peak, we had a kid here and there.”
In total, nine children were hospitalized as of Aug. 12. None were vaccinated, although some were eligible, Jimenez said. As children head back to school, he strongly recommends all children aged 12 and older get vaccinated.
“If a child gets COVID, we can’t today be so confident that they’re not going to wind up in the hospital — let alone sick,” Jimenez said.
Some parents have voiced concerns over the Food and Drug Administration's emergency use authorization, but scientists say it’s simply a procedural delay and already know the vaccines are safe, Jimenez said.
While Shands is not at capacity like other Florida hospitals such as Lake City Medical Center, Jimenez said when outlying communities look to Gainesville hospitals for support, it creates a spillover of patients.
“Hospitals in our periphery are getting overrun with COVID,” Jimenez said. “When that happens, it puts pressure on the hospitals in Gainesville.”
About half of the COVID-19 patients at Shands are not from Alachua County, Jimenez said.
Although not every patient has the Delta variant, Jimenez said more sequencing is revealing more patients with the variant, leading to the conclusion that the outbreak is likely Delta related.
Emerging Pathogens Institute developed the projected COVID-19 model, estimated by UF researchers Ira Longini and Thomas Hladish and updated on Aug. 14, that predicts the peak in the Delta surge for Florida to be in late August and early September.
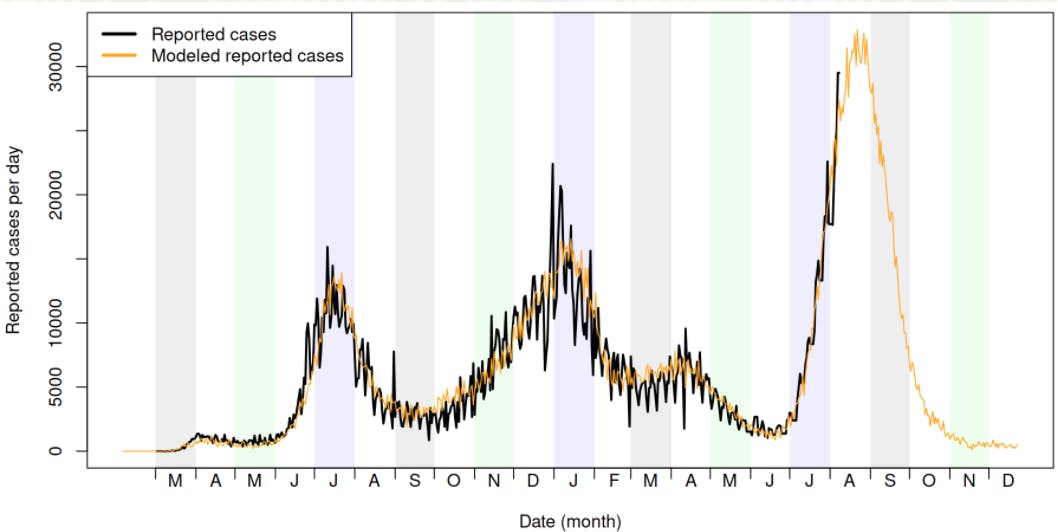
UF Emerging Pathogens Institute and others modeled a projection of reported daily cases for Florida with a peak of 33,000 cases per day around late August and September.
The report also predicted a peak of about 60,000 symptomatic and asymptomatic infections per day. With changes in testing availability and lags in reporting, the report states the infection curve looks significantly different than the reported case curve.
The report detailed death estimations, which are likely to peak substantially after the peak in reported cases. Jimenez said hospitalizations also tend to lag behind infections.
The prediction is based on a transmission model that includes people from different demographics and households in Florida, Hladish said. The model factors in the different lifestyles of residents, new variants and the vaccination campaign in order to accurately simulate transmission.
“This is by far the worst that we’ve had in terms of how many people are infected and how rapidly it has spread,” Hladish said. “This is a much more infectious variant.”
The health care system is overwhelmed and stretched thin due to these surges, and the consequence goes beyond people with COVID-19, Hladish said.
“COVID is not the only reason that people go to the hospital,” Hladish said.
With this spike in COVID-19 patients affecting the access to care for every patient, first responders are also starting to feel the weight of these consequences that Hladish mentions.
“Last year, if you had said COVID was a hurricane, we did warnings, and we evacuated people, and we took all these precautions to minimize the damage of the hurricane,” said Harold Theus, fire chief of Alachua County Fire Rescue. “This year, the hurricane just hit us without any warning.”
In mid-July of this year, the daily number of transports was increasing, Theus said, and the wait time for a bed to be transferred to increased, as well.
On average, first responders typically waited for 15 to 30 minutes, Theus said. The end of July saw a huge increase in wait times, with some rescues waiting anywhere from one to sometimes three hours.
Because these first responders spent so much time waiting, it caused a shortage in available help for incoming 911 calls.
Alachua County Fire Rescue, on average, transports 85 patients a day, Theus said. Right now, they have been reaching 95 transport calls a day.
“What’s happening now is we are managing the call load — it’s happening — we’re having good quick responses to all of our calls, but it does certainly create a lot of fatigue on our crews,” Theus said. “Each call, they [first responders] have to think about this communicable virus... ‘I hope I’m not exposing myself to getting this virus and my family.’”
Theus said the stress of making sure to stay safe is taking a tremendous toll on all their first responders.
“Be patient and think of our health care workers,” he said. “Obviously, our thoughts and prayers are with the sick and with the COVID families, but it is also taking a tremendous toll on our EMS workers and our hospital staff.”
Shands staff are also exhausted and worn thin, Jimenez said. For 18 months, there has not been a single day at the hospital without COVID-19 patients.
While Shands is not mandating vaccines, Jimenez said any employee who is not vaccinated will have to wear an N95 mask starting this week.
Jimenez said he asked one of the nurses how he was doing, and he told Jimenez he’s okay. But then his voice trailed off.
The nurse told Jimenez he knows when a patient is headed toward death. Separated by glass panels, the nurse calls in a family member for one final goodbye.
“It gave me shivers,” Jimenez said. “My goodness, imagine being a nurse having to witness that — not just once, twice or three times.”
Other staff expressed to Jimenez an unsettling sense of déjà vu.
“‘This is Groundhog Day again,’” he said. “‘How did we let ourselves as a society get back here?’”
Contact Alexandra Harris at aharris@alligator.org. Follow her on Twitter @harris_alex_m.
Contact Elena Barrera at ebarrera@alligator.org. Follow her on Twitter @elenabarreraaa.

Alexandra is a senior journalism major reporting on Science/Environment for The Alligator. Her work has appeared in The Gainesville Sun, and she filed public records requests for the Why Don't We Know investigative podcast. She has a passion for the environment.

Elena is a second-year journalism major with a minor in health sciences. She is currently the University Administration reporter for The Alligator. When she is not writing, Elena loves to work out, go to the beach and spend time with her friends and family.






